Core
Gluteus Medius
Calves
Quads
Gluteus Maximum and Hamstrings
Core
Gluteus Medius
Calves
Quads
Gluteus Maximum and Hamstrings
If your shoulder gradually begins to lock up on you, making most movements painful and stiff, there's a chance you are dealing with frozen shoulder. Otherwise known as adhesive capsulitis, this condition often comes on out of the blue, although it can also occur after a trauma like a fall or surgery. This can be a very frustrating condition that mostly affects women between 45-65 years of age and can last 9 -24 months. But knowing how to treat it can greatly reduce the time you spend in pain and dysfunction, and even help you avoid painful or risky procedures. Fortunately, some very recent studies help shed some light on what works best.
First, a little more background on this unique shoulder condition.
Frozen shoulder occurs when the shoulder capsule starts sticking to itself. This prevents the capsule from extending, causing pain and a gradual restriction in range of motion. Treating this condition is a big challenge and diagnosing it is even more challenging.
But going through it is the real problem for several reasons. First, it can be frustrating having a condition where you often don't know how or why it developed. Second, knowing the condition can limit you for up to a year can be daunting. Third, suggestions for treatment vary between surgery to physical therapy, to doing nothing.

Fortunately, there is an excellent landmark study published recently that for the first time compares the most common treatments for frozen shoulder to see what works. Researchers in the UK designed a randomized control study to compare surgery (capsular release) plus PT, manipulation under anesthesia plus PT, and 12 Weeks of PT only for treating adhesive capsulitis. All participants also had a cortisone injection.
At 12 months, there were no differences in outcomes: all groups had improved to achieve the same level of function and pain. However, several people in the surgery and manipulation group experienced adverse effects, while none in the PT group did. Thus, PT was just as effective and lower risk compared to the other treatments. (Rangan A, et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicenter, pragmatic, three-arm, superiority randomized clinical trial. Lancet. 2020 Oct 3). While many studies have shown PT to be effective, and some in combination with an injection, this is the first to directly compare PT with surgery or manipulation.
This provides some clarity to what can seem to be a murky situation for those trying to decide what is the best course of action to fix their frozen shoulder. The recent evidence supports what I have seen in the clinic and what other research has shown: using physical therapy alone is likely the best way to fix frozen shoulder.
But there is another vital reason to start with physical therapy: the diagnosis. Determining whether you have frozen shoulder in the first place is a huge challenge for even the most experienced shoulder specialist.
Fortunately, my colleagues have an unusually high amount of experience diagnosing adhesive capsulitis. This is partly due to seeing it dozens of times over the last couple decades and knowing what to look for. But it is also due to an important luxury uniquely afforded to PTs versus other practitioners: Time!

PTs have more time to do an involved exam, plus we can repeat it several times a week and assess reactions to treatment. This is important because it is really difficult to get a proper diagnosis in just one 20-minute exam. Adhesive capsulitis can present with similar findings as other conditions, such as rotator cuff tears or cervical radiculopathy.
And imaging like x-rays and MRI can make things even more complicated. Such imagining will often show arthritis and tears in over 50% of people that don't have any pain or limitation so it's possible that someone with adhesive capsulitis will be misdiagnosed as a rotator cuff tear. This could be a big problem, leading to someone undergoing a surgery to "fix" something that wasn't a problem in the first place. Also, frozen shoulder plus rotator cuff rehabilitation is quite painful and difficult. In fact, surgery can often trigger one type of frozen shoulder (secondary adhesive capsulitis). One of the distinguishing factors of frozen shoulder is that the pattern of range of motion restriction is unique.
For example, most with frozen shoulder will be restricted with internal rotation (reaching your bra strap), external rotation (reaching the seat belt), and reaching out to the side. This limitation is found with both passive AND active motion as the rotator cuff is not the cause of the problem. Another distinguishing factor is that strength remains relatively high and pain free in the early phases in those with frozen shoulder.
In contrast, those with rotator cuff issues will have greater passive motion. This is because the rotator cuff is involved in active motion but does not restrict passive motion. Also, those with rotator cuff problems test as weak and painful as the irritated rotator cuff is not able to produce normal force.
Cervical problems can be differentiated from adhesive capsulitis as movements of the neck will reproduce the shoulder pain and a neuro exam will often reveal deficits. Several other factors in a thorough exam performed by a specialist in both cervical and shoulder disorders will distinguish a frozen shoulder from these conditions.
So, it is very important to get the diagnosis right, and the best environment to do so is during PT. At the very least, you can learn some important self-management strategies about frozen shoulder and become informed about what to expect from this condition. At best, and most likely, PT will resolve the condition completely. The good news is that, in our experience, frozen shoulder can resolve in a much shorter timeline with proper PT compared to the usual 9-24 months. Also, no matter what treatment you pursue, full recovery is very likely.
But there is a very important distinction between treatment options that rarely is discussed: preserving strength of the involved arm as well as health and fitness of the rest of the body.
Unfortunately, many are led to believe that when they have frozen shoulder, they should rest and protect that arm, and by association, avoid upper body exercise. Evidence shows that this is not the case. In fact, adding rotator strengthening exercises to the effected arm resulted in superior outcomes compared to those who did not. (Rawat P, et al. Effect of rotator cuff strengthening as an adjunct to standard care in subjects with adhesive capsulitis: A randomized controlled trial. J Hand Ther. 2017 Jul-Sep;30 Also, dozens of studies have proven that training the unaffected arm will have positive effects on the effected arm. This is known as the cross over effect. While one arm may be strong or tolerate more range of motion, both arms should be trained, and can be trained separately to accommodate for these differences.
For example, instead of a pushup, you can do a 1 arm dumbbell press with separate weights. Or instead of a pull down with a bar, you can do single arm pull downs with a handle. And of course, all aerobic, core, and lower body exercises can be modified and should be continued.
Having some help with making these modifications and encouraging continued participation with a comprehensive exercise program is a vital, but often forgotten advantage of seeking physical therapy care compared to all other options. Too often, the pain and inconvenience of an orthopedic problem is compounded by the side effects of general deconditioning. This can be avoided with proper physical therapy care.
Here's What To Do If You Think You Might Have a Frozen Shoulder:
Reach out if you suspect you have adhesive capsulitis to get proper treatment by clicking here.
If you have already had physical therapy for frozen shoulder and are looking to get your arm strong again without getting hurt, click here.
Chances are you or someone you know has dealt with sciatica. This is a condition when you have pain; be it sharp, dull, or tingling, that shoots from your rear, down the back of your thigh, or down your leg.
Unfortunately, this condition is poorly managed. As a result, it needlessly wreaks havoc on people's function, fitness, and can contribute to unnecessary pain, disability and exposure to risky treatments.
The usual treatment for this condition is all over the place:
However, these treatments are not usually effective or supported by the evidence. And a recent study further clarifies this.
The evidence shows that physical therapy consisting of exercise and manual therapy is significantly more effective.
Before we delve into the evidence and best treatment options, let's get a deeper understanding of sciatica.
What is sciatica?
Sciatica refers to a condition that causes pain from your low back to your buttock, posterior thigh, and leg. These symptoms are attributed to an irritation of the largest nerve of the body, the sciatic nerve. This irritation can be from inflammation, compression, or excessive tension applied to the nerve.
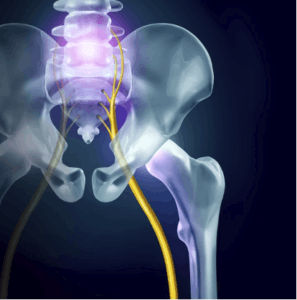
Damage to structures adjacent to the sciatic nerve or its associated nerve roots, such as spinal structures or hip muscles, are suspected culprits for contributing to the nerve irritation. However, this is conjecture, and no imagine can confirm the exact mechanism of the irritation. This partly explains why approaches trying to target a specific part of the anatomy have very poor success rates.
It's quite a frustrating condition that can linger for weeks or months without proper treatment and can wreak havoc on your function and fitness goals.
What's the first thing to do if you have Sciatica? The Recent Evidence
Researchers recently investigated whether the usual course of care or physical therapy was more effective in treating sciatica. 220 people presenting to a primary care setting with sciatica lasting less than 90 days were randomly assigned to one of 2 groups. Group one received the usual care, which involved education and medication (anti-inflammatories and muscle relaxants).
The other group received 4 weeks of physical therapy, which consisted of exercise and manual therapy. At 4 weeks, the physical therapy group demonstrated superior outcomes. 1 year later, the physical therapy group continued to show lower levels of pain and disability. Fritz, JM et al. Physical Therapy Referral From Primary Care for Acute Back Pain With Sciatica A Randomized Controlled Trial. Annals of Internal Medicine. Oct 2020.
These findings tell us what my colleagues and I have known from treating hundreds of patients with sciatica: those who get physical therapy do better than managing it with medication. And the earlier sciatica patients receive PT, the better.
How to Fix Sciatica
Here are the steps I have found, based on the evidence, being a patient with sciatica, and treating hundreds of patients with sciatica for the last 2 decades has been most effective in fixing sciatica;
1. Make a PT appointment
The research above confirms what other studies have found: early PT improves outcomes. Evidence also shows that early PT also lowers the risk of surgery, reduces costs, and lowers the likelihood of using addictive pain killers. But there is another important benefit: getting a proper diagnosis. Sciatica, like many back issues, can be difficult to diagnose. No matter how skilled the clinician, having only 15-30 minutes on one day to evaluate a condition is challenging. In contrast, seeing how your condition responds over time on different days to various movements and treatments is essential to confirm a diagnosis. This is not possible in environments other than physical therapy, where you are seeing a Doctoral trained clinician for 30-60 minutes several times a week.
We can gather critical information to make sure we are treating the right condition. For example, many people have been sent to me with a diagnosis for calf muscle strains, hamstring injury, or knee arthritis, only to find out that upon PT examination these were sciatica cases. In other situations, we've seen people referred to us for sciatica and low back pain that were not responding as expected to treatment and examination revealed inconsistent findings.
This information allows us to send the patient back to his PCP with justification to explore non- orthopedic causes of their pain. In 2 such instances, it was determined that their back and leg pain was referred from having kidney stones. The most supported PT treatment involves exercise, manual therapy, and education. Thus, PT's who specialize in this treatment approach, versus passive modalities only (e-stim, ultrasound, stretching) are best to treat sciatica.
2. Stop stretching.
One of the biggest mistakes in treating sciatica involves stretching the hamstrings. Nearly all sciatica patients that I'm seeing as a second opinion due to failure to respond to prior treatment notice that their pain improves within days with advice to stop stretching their hamstrings. Because the hamstrings are often tight and are located near the path of the sciatic nerve in the back of the thigh, many clinicians and patients alike believe that this tightness is causing their sciatica. Accordingly, they think stretching the hamstring will help. However, this often makes it worse because muscle and nerve react quite differently. While a muscle will tolerate stretching quite well, an irritated nerve will not.
Doing so is like adding gas on a fire. While some may report that stretching actually feels good, this is only temporary and can create a vicious cycle. The sense of stretch may create a diversionary symptom that drowns out the sciatic symptoms, but then later return and the hamstring muscles often tighten as a guarding response. This is similar to stretching an itch: it may provide temporary relief, but it often causes skin breakdown and elevates histamine that fuels the itching sensation. This is similar to stretching the piriformis, a hip muscle that is located near the sciatic nerve as it passes the buttocks.

In about 20% of the population, the sciatic nerve passes straight through the piriformis muscle. Somehow, this has led clinicians to suggest stretching the piriformis to treat sciatica. However, a close look at the mechanics of the piriformis stretch would reveal that stretching this muscle would add tension and compression to the nerve, as opposed to relieving it. Also, there is no proof that piriformis tightness, nor stretching that muscle, relieves sciatic symptoms.
Given that both of these suggestions lack support and have a high likelihood of worsening symptoms, avoiding these stretches when the sciatic nerve is irritated is an excellent first step. While these stretches may be tolerated later as the sciatic nerve calms down, doing so while the nerve is aggravated is not advised.
3. Change ergonomics
Given that prolonged tension or compression on an irritated nerve will often prolong irritation, these positions need to be identified, then modified or avoided. Common positions are sitting up in bed or sitting with the feet elevated on an ottoman. These positions increase the tension of the sciatic nerve and will often flare up symptoms. Sometimes prolonged standing will also aggravate sciatica, which is common when there are sensitivities to compression. This is best modified by doing intermittent traction while standing, weight shifting, or minimizing uninterrupted prolonged standing.
4. Make a provocation/Alleviation list
Knowing exactly what increases your symptoms and decreases your symptoms is vital information. Having it in list form can make a seemingly mysterious condition appear much more manageable. This serves as your reminder for what you need to address in order to solve your sciatica condition. If you do the correct treatments but fail to change the thing that are making your pain worse, it can be like taking Tylenol for a headache, then banging your head on a wall.
5. Make a modify/avoid/do list
This directly relates to the above. For the things that you have identified as provoking your pain, you need to decide if you can avoid them until things calm down or not. If you can avoid them, then do so. But if these things are unavoidable, then they need to be modified. For example, if sitting provokes your pain, but you need to sit for work or commuting, then change your chair, take more frequent standing breaks, or do intermittent deloading while you sit. These are the things that get overlooked in treatment, but probably make the biggest difference in outcomes.
6. Get a neuro exam
If a nerve root is affected as it exits the spinal column, its function can be compromised. While symptoms radiating down the leg may be one clue that the nerve may be affected, it is not a very reliable finding. This is because irritation of several other structures of the spine may also refer pain down the leg. Imaging, such as MRI, is also a flawed way to determine the involvement of nerve irritation, as many people without any pain or dysfunction have MRI findings of herniation or "nerve compression".

However, a neuro exam may be a better indicator of the status of how the nerve roots as they exit the lower lumbar spine are functioning. A neuro exam involves testing three important functions of a nerve root: motor (strength), sensation (touch, temperature), and reflexes. Each nerve root is responsible for the function of specific muscles (myotomes), area of skin (dermatome), and specific reflex (Deep tendon reflex). This is really important as it can identify if a nerve root is involved, how severe the involvement is, and whether it is improving or not over time. For example, if a patient presents with weakness of his tibialis anterior (the muscle that pulls your foot up), decreased sensation on the inside of the shin, and a diminished patella reflex, then it is likely that the L4 nerve root is affected.
If these signs become more severe over time, it increases the rationale to consider more aggressive treatment to prevent permanent nerve damage. While this is rare, it is vital and may prevent permanent impairment. Conversely, improvements in the neuro exam findings, even in the absence of improved pain, can serve as a positive indicator of potential for future improvements. This is important as it can prevent people from giving up on conservative treatment or seek risky and unnecessary treatment.
While many clinicians do rough neurological assessments (having you walk on your toes, then heals, then hitting your patella with a reflex hammer) a thorough neuro exam is more involved and uses a grading system to detect more nuanced changes. Also, a neuro exam should be done not just once, but several times as the condition may change and detecting these changes early are important. A physical therapist with residency or fellowship training in spine care is best to perform a neuro exam, as they have the training and time to perform more frequent and thorough neuro exams.
7. Determine sensitivity to tension, position, or load.
Understanding your sensitivity to these 3 things will greatly help guide treatment and resolution of your sciatica. This is best done during a PT exam. Tension sensitivity: tests that evaluate the response of the nerve tissue to stretch can help make the diagnosis more accurate. For example, a slump test may help distinguish between a hamstring injury versus sciatic nerve irritation. It can also help measure the rate of improvement and guide decisions about when to resume normal activity.
Position sensitivity can help determine which activities to modify or avoid, and which type of exercises to pursue. This can make or break the success of treatment.
Finally, assessing load sensitivity can be critical for acutely reducing symptoms, and may hasten recovery. For example, if a patient is determined to be load sensitive, doing traction in the clinic and teaching you how to perform self-traction can be the difference between a bad day in pain versus getting significant relief. Some evidence indicates it may improve the fluid dynamics and nutrition of the disc as well.
8. Identify risk factors
Individual risk factors that you can modify may make you at risk for various back problems, and thus could be contributing to the cause of your back pain. Finding these risk factors and improving them can be important for not only recovering from sciatica, but also for preventing it from coming back. For example, impairments with motor control, endurance, strength, mobility, and general fitness can be contributing factors that are easily improved with proper care.
9. Understand pain
Too many people fear pain or ignore pain. Both extremes are rarely successful. Understanding what pain is can greatly improve your ability to manage your sciatica. For example, knowing that the severity of pain does not always correlate with the severity of damage can prevent you from pursuing unnecessary, ineffective, or dangerous treatments. Pain education is a critical element of proper treatment.
10. Stay Active

It may sound counterintuitive, but one of the most important things to do when you have any back condition is to remain active, as complete rest has been proven to negatively effect outcomes. The trick is to figure out the right type and amount of activity. Too much of the wrong things will aggravate the condition, and too little will do the same through increasing tissue sensitivity and lowering resilience. We need to find the "goldilocks zone".
Staying active will not only help your condition improve, but it is absolutely vital for your general physical and mental health. An injury is a reason to move, not a reason not to move. The key is finding the right type and amount. As a patient, it is hard to be objective about this, thus, having the support of a clinician is key.
What to do next
Get help from a trained clinician with experience in treating and preventing back problems if you have been dealing with sciatica symptoms. In most cases, this means seeing a residency or fellowship trained physical therapist. Click here to schedule an exam, or learn more about our clinicians. If you aren't in the area, this can at least give you an idea of the background that I would look for when choosing a PT.
A personal trainer or fitness coach experienced in working with post-rehabilitation will also be a good resource. Especially if you have had chronic back or sciatica problems that have been successfully managed in PT, but you would like to get in better shape and aren't sure what you can do without provoking your back problem. Click here to set up a consultation.
Sciatica can be a frustrating condition and having so many different treatment options and opinions can make it more challenging. Fortunately, focusing on the evidence and following success clues from the clinic is a good reason to be optimistic for a full recovery. Hopefully the information above gives you some good first steps as to what to do to help your sciatica!
Are you in constant or recurring pain that will not let you enjoy your life as you would like? Do you suffer from the effects of an old injury, a degenerative condition, or some other situation that calls for ongoing pain management? If so, then your first instinct might be to reach for medication — but hold that thought, because drugs can pose their own threats to your health. Physical therapy can provide safer, effective, non-addictive, long-lasting strategies to manage pain.

Drugs promise quick (if only temporary) relief from many kinds of pain. Unfortunately, they can harm as well as help. The most glaring example is the addictive potential of opioid drugs. Opioid dependence and abuse have become a national nightmare in the last decade. The CDC estimates the total economic burden of prescription opioid misuse alone in the US is $78.5 billion/year including the costs of healthcare, lost productivity, addiction treatment and criminal justice involvement. Some researchers even feel that many people who would otherwise be able to work are sidelined because they would fail a drug test. Roughly 21-29% of patients prescribed opioids for chronic pain misuse them. Between 8-12% develop an opioid use disorder. An estimated 4-6 % who misuse prescription opioids transition to heroin. As mind-blowing as these numbers are, to a person who uses prescription pain medication for pain relief, opioids may seem like the path of quick recovery. The misuse of opioids remains a problem in our society. The key is to seek help before pain gets out of control.
Even over-the-counter pain relievers can pose dangers to your health. Taking painkillers to rid yourself of pain may seem like a good solution, but it is not. Over-the-counter meds like aspirin, ibuprofen and acetaminophen can have side effects. Taking a lot of aspirin can cause your stomach to bleed and can also cause kidney damage. Acetaminophen can result in kidney damage. Ibuprofen can cause both kidney and stomach problems. Not only does taking meds for pain just mask the problem, it may cause you another one. Using medication for pain does not get to the root of the problem. None of these medications are meant to be used long term. Pain is not supposed to linger.
Pain is your body’s natural warning system — which makes it a particularly important and useful communication tool at early onset of injury. Nerve signals alert you to a problem that requires attention, from an infected area or traumatic injury to joint or overuse of a muscle or tendon. This is especially true of acute pain. Sensations of pain and stiffness discourage you from using an injured body part while it is healing; once the condition resolves, pain should go away.
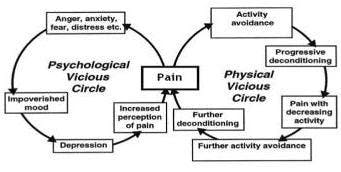
When pain does not go away, it is important to investigate why. Sometimes pain will outlive its usefulness, lingering on for months or even years after your body has done all it can to address the underlying problem. We call this chronic pain. It afflicts some 116 million people in the U.S. alone, that is 1 in 10 people suffer from chronic pain. The pain may plague you constantly, or it may come and go in bouts that last for weeks at a time. We have a quick fix culture and physicians yield to meeting patient’s demands for passive prescriptive treatments. The solution is not to repeatedly mask pain with medication and put off the need to address why your body is trying to tell you something. Pain and suffering are the primary reason American’s are on disability. This vicious cycle is because the root causes of pain are left unaddressed. As the opioid epidemic has inflicted the US and healthcare professionals are seriously reevaluating its abuse, it is worth noting that PT has long been considered a safer, cheaper, and more effective treatment for chronic pain.
Physical therapy not only can help relieve pain; it addresses what is causing the pain in the first place. A physical therapist is a highly trained medical professional, and an expert in the biomechanics of movement. Through advanced diagnostic procedures, a physical therapist can uncover the source of your pain and find ways to address it for long-term health and mobility. Our healthcare mindset needs to shift. Physical Therapy should be a first line response to pain. A physician will outsource your needs, whereas a PT will help you take charge of your own care.
The focus of treatment should be to restore function disability not just treat pain symptoms alone. This would make the 1/3 US population much more productive and living a better life without paying the price of drugs. Physical Therapists are in a prime position to guide a person who is suffering from pain, disability and struggling with the social, psychological, and even economical stressors that accompany pain. Treatment addresses the physical and psychological challenges a patient is faced with when trying to get their life back. Clinicians address a patient’s individual concerns and apprehensions with weekly support and coaching, keeping a person on track with necessary lifestyle changes that will empower an individual to take control of pain while restoring physical function. Careful exposure to exercise and activity while keeping symptoms at a minimum permits a person to discover how physical activity can be a path and even the reward to relieve pain.
Stay tuned for additional information about the integrative science of pain. If you’ve ever experienced a disabling injury it would behoove you to know what is the difference between acute and chronic pain, learn about the psychological components of chronic pain, and discover how a person who has learned how to avoid physical activity because of pain, can take control over pain and return to a more productive life.

If you are a runner, you are probably overjoyed by the fact that you are still able to safely run during the COVD-19 pandemic. Not only are you able to run, you are actually encouraged to do so as it is important not just for your fitness, but also your immune and mental health.
Your running, however, has probably changed:
While running is still allowed, it has changed.
“It is not the strongest of the species that survives, nor the most intelligent that survives. It is the one that is most adaptable to change.”
-Charles Darwin
With all of the current changes to your running, this may be a perfect opportunity for you to make additional adaptations to not just survive, but to thrive.
If you have a chronic, low grade injury that tends to flare up with an increase in intensity or mileage, this may be the time to do something about it.
Maybe you’ve always wanted to learn how to become a more efficient or faster runner?
Possibly you’ve heard that you should be doing strength training but you’re just not sure what you should be doing.
Luckily for you, OP is here to help.

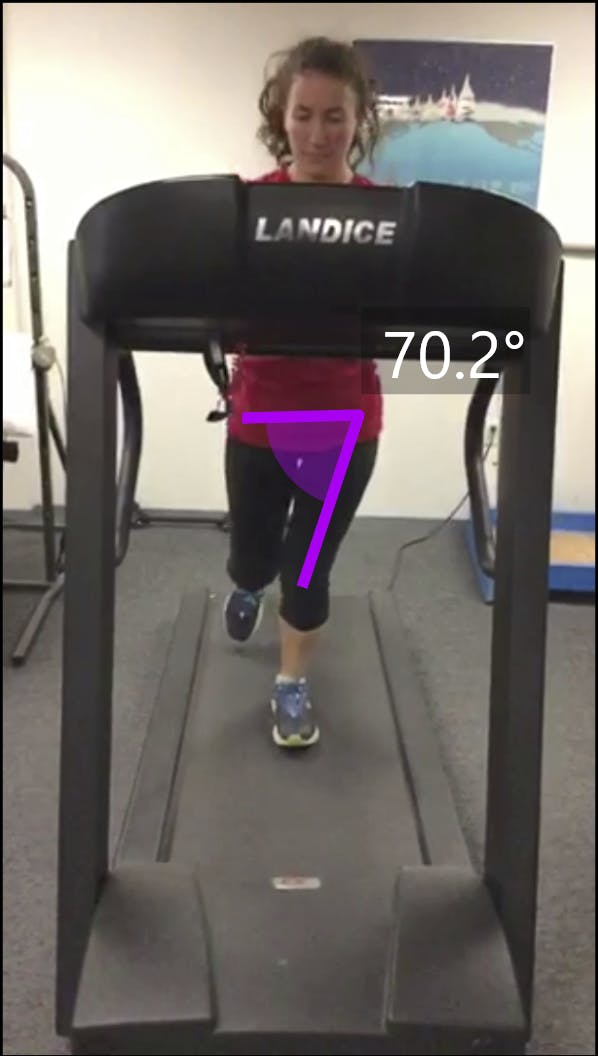
Through Limitless Running, we have both in-clinic and virtual options to perform a gait analysis that will identify the problem areas in your running form. With follow up visits including gait retraining to correct your form and a re-assessment to ensure that you are on the right track, we’ll be able to help you get back to running without injury and with improved efficiency.
Our highly trained physical therapists are also runners who enjoy spending their free time geeking out over the optimal knee bend during initial contact and what percent of running cadence increase has been shown to be most beneficial in the newest systematic review. They have a plethora of information to share with you and encourage you to pick their brains.
If you would like to learn more about our new program, head to our webpage here.
Quick Facts:
From my experience, both as a long distance runner and a physical therapist, getting runners to perform strength training is similar to getting a picky 3 year old to eat raw broccoli. Not easy. Personally, I do not enjoy strength training. Tell me to go spend 5 hours alone on a technical trail in 40 deg weather with pouring rain and gusting wind – no problem. Ask me to spend a total of two sessions in a gym per week and I will revert back to my 3 year old self and stare you right in the eye as I intentionally drop my broccoli onto the floor.
Based on these opinions, I was excited to read an article by the PT running goddess, Irene Davis, that explained that strengthening, specifically hip strengthening, has no effect on running form. Her article demonstrated that although strengthening the hips of runners with poor form improves hip strength (obviously) and performance of a single leg squat (similar to landing position of running), there was no change in the participant’s running pattern. After reading this, I smiled, high fived myself, and began dreaming of a life without gym bros. Kidding.
Then why strengthen?

While Willy & Davis, Feber, and Earl & Hoch, have demonstrated that just strength training alone is not enough to improve poor running form, strengthening does have its place in the world of running. Most notably, it can do wonders for preventing injury and making you faster. If you strength train (and eat your raw broccoli), you’ll never be injured again and you will win all of your races. Kidding again.
Realistically, strength, or lack thereof, has been shown through a plethora of studies to be associated with injury rates. A too-close-to-home one includes a systematic review that demonstrates that females with patellofemoral knee pain (generalized front of the knee pain) are found to have weaker hips. This corresponds with other studies that demonstrate that females with patellofemoral knee pain are found to run with aberrant hip mechanics such as this:
The working theory is that weakness will lead to faulty gait mechanics (running form) which will then lead to injury. Pretty solid.
Why, then, is just strengthening often not enough? If we get stronger, shouldn’t our gait mechanics also improve?
If only it were that easy. Research has been able to clearly demonstrate that weakness can lead to poor running form which can lead to injury, but once those running mechanics become our new pattern, they are not easily changed.
Think back to your most recent vacation. Without an early morning work meeting requiring you to set an alarm, you may have gone to bed a little later than usual on the first night smiling at the fact that you get to sleep in. As the vacation continued, that bedtime probably crept further into the night and that sun continued to rise higher in the sky before you opened your eyes. All was well and good until back-to-reality Monday morning hit and you had to hit snooze three times and lower your personal hygiene standards in order to make it into work on time. Falling into that new sleeping schedule was easy, climbing back out of it – bit of a challenge.
Just as it often takes different and more difficult steps to revert back to your normal sleep schedule after a vacation of late nights, improving your gait mechanics after injury requires a bit of effort. Strengthening will help. Specific drills and strategies to improve running form can assist. But just as Davis demonstrated, we need more than that.
We need gait retraining.

Gait retraining is simply an umbrella term used to describe ways in which we can change running form and it has been shown time and time again to improve your running pattern, rid yourself of injury, decrease total load on your joints, and increase your performance. Gait retraining typically falls into two different categories, visual and auditory. Visual gait retraining can include placing a mirror in front of your treadmill to watch yourself run with special markers and tricks. Auditory retraining is very commonly prescribed as running to a metronome or listening to the sound of your footfalls (with specialized equipment). While some of these tools may be helpful to you, determining which one will help and how to use it appropriately needs to be prescribed by a medical practitioner who is trained in performing a gait analysis. This is a PLEASE REACH OUT TO AN EXPERT warning with a caveat that knowledge is power so you can also learn more about gait retraining here.
During the COVID pandemic, we are currently offering in-clinic and virtual gait analysis with assessment and follow up sessions to safely and effectively provide gait retraining to injured runners. If you are interested in learning more, please click here for more help or give us a call at 978-927-0907

Quick facts:
When you feel that faint tug on your kneecap as you descend a set of stairs after a challenging run, are you haunted by that whisper in your ear, “running is bad for your knees?” As an ultra runner and physical therapist, that voice in my head has been strengthened by numerous friends, family members, and even patients who try to warn me that I’ll be facing a world of pain when I’m older if I keep up this “crazy running” thing.
My reply is generally two fold:
Well, fortunately and unfortunately (who likes to be wrong?), I have been responding incorrectly. My “educated decision” did not include new evidence that has emerged indicating that not only is running not related to knee osteoarthitis, it may actually be protective for your knees.
Here’s the old thought process: Running involves a lot of pounding, pounding causes damage, therefore, by the transitive property, running causes damage. Don’t worry, I’m not making an argument against the transitive property (it’s maybe the only part of geometry that I remember from Mr. Lindahl so I’m holding onto it), I’m just no longer convinced that pounding causes damage.
“Damage” or degradation of the cartilage in your knee leads to osteoarthritis. Signs of osteoarthritis can be determined by a few different mechanisms, two of them being the level of cytokines and COMP in your synovial fluid. Okay, okay, let’s back up and define. Your synovial fluid is the fluid inside all of your joints that provides nutritional support for your cartilage and reduces friction. This synovial fluid contains COMP or cartilage oligomeric matrix protein that is a marker for worsening osteoarthritis. This fluid also contains cytokines which are proteins secreted by the immune system that are a sign of inflammation, which is chronically high in patients with osteoarthritis. Basically, high levels of COMP and cytokines are bad news for your knees.

Based on the old thought process, one would expect that runners have relatively higher amounts of COMP and cytokines in their knee joint synovial fluid because people assume that running causes osteoarthritis. However, a new study conducted out of Provo, Utah looked at these two proteins, COMP and cytokines, in volunteers after they had been sitting for 30 minutes or running for thirty minutes. To the glee of all runners, this study found that the levels were HIGHER than baseline in the volunteers after they had been sitting and LOWER than baseline values after they had been running.
Therefore, running may actually protect your knees from osteoarthritis.
Before you text an “I told you so” to all of those NARPs (non-athletic regular person) who have ever questioned your running obsession as you throw on your running shoes and race out the door, here are a few things to keep in mind:

While no other studies solve these issues with analysis of COMP and cytokine levels, luckily, these are not the only scientists who have studied osteoarthritis and running. An article from 2009 looked at long-distance runners over the age of 50 who had already been running for about a decade and matched them with similarly aged participants who did not run. After Xraying these folks every few years for the next decade, there was no difference in the acceleration, prevalence, or severity of osteoarthritis between those who ran and those who didn’t. In fact, the only knee replacements that were performed between these 98 participants were non runners. PLEASE do not infer from that statement that no runner will ever require a knee replacement.
Other grains of salt regarding that study include that the runners group had a lower BMI (higher BMI is associated with increased risk of osteoarthritis), were slightly younger, and had a greater prevalence of prior knee injuries. While all of these values were statistically non-significant, (i.e. age of runners: 59.8 vs age of controls: 60.2), they should be kept in mind. Another key quality of the study to consider is that osteoarthritis was determined through radiographic imaging, yet we have a ton of evidence that demonstrates that Xrays do not always correlate with symptoms. Just because a runner’s Xray doesn’t look too shabby, doesn’t mean that runner is pain free in the knees.

While, as always, more studies should be conducted to look at the long term effect of running on knee OA, I’ll leave you with some statements from oldie but goodie articles:
“Our observations suggest, within the limits of our study, that long-duration, high-mileage running need not be associated with premature degenerative joint disease in the lower extremities”
And
“In sum, habitual physical activity does not increase the risk of knee OA for men or women.”
I’ll make sure to hear these voices in my head next time my knee complains on a stair 🙂
If you want to learn more, click here

Quick Facts:
As spring weather begins to tease with occasional days of sunshine and warmth, the call to run in the great outdoors reaches its peak. After experiencing a run filled with breathing in your own hot phlegm that’s stuck to your mask and dodging the newcomers who have discovered your favorite running route, you may find yourself opting for indoor exercise and instead, pumping out seemingly endless miles on a dreadmill – sorry, sorry, treadmill. While this can allow you to get in a solid training run devoid of any potential pandemic threat, there are a lot of questions surrounding the belted beast. Will running on a treadmill vs running outside change your form? Is the old 1% incline rule real? Why is it so freakin’ hard?
Will running on a treadmill vs running outside change your form?
A bit. Does it matter? Not so much. KINETICally speaking (think force or load on joints), there is a slight difference in the amount of load on your muscles and tendons as you run on a treadmill versus running outside. A recent study shows that your quadriceps muscles can work as much as 27% LESS on a treadmill versus outside, formally called overground. If you are training for a (likely virtual) hilly race, make sure you supplement your treadmill training with some eccentric quadricep training to prevent quad explosion on the downhills. On the flip side, your achilles tendon (the thick tendon that connects your calf muscle to the back of your heel) undergoes up to a 14.2% increase in stress on the treadmill versus the great outdoors. If you suspect that you’ll be spending a chunk of this pandemic on a treadmill, make sure to get your achilles ready with some calf raises.

How else does your running form change? KINEMATICally speaking (think position of joints, not force), your hips, knees, and ankles hit pretty much the same angles when you run on a treadmill versus overground. A recent – excuse me – very recent, meta-analysis found that the only difference on treadmills is that when your foot hits the ground, your toes tend to land a little closer to the ground (less dorsiflexion) and your knee has a bit more bend (more flexion). This corresponds with a step length difference of 1-5% which generally indicates that your initial contact (when your foot hits the ground) is closer towards your center of mass (more underneath your body). PHEW. Just look at the pictures.

Fine? Better!
Except that they suck. I don’t think I am alone in feeling as though each mile run on a treadmill deserves a medal in itself as the miles – no – the 0.1 miles, tick by ever so slowly.
So is running actually more difficult on a treadmill?
No. In reality, according to a commonly cited , if you are running anything faster than a 7 minute mile, you should actually increase the treadmill to 1% incline to make up for the lack of air resistance. And if you can get up to around a 5 minute mile, you may even want to increase it to 2%. Yikes.
Despite the fact that running on a treadmill requires less energy due to the lack of air resistance, this meta-analysis found that when running at faster speeds, your heart rate and perceived level of exertion are higher on a treadmill than if you are running that same fast speed overground. Conversely, when running at slower speeds, your perceived level of exertion and your heart rate are decreased on a treadmill versus running that same slow seed outdoors. Kinda weird. We can only speculate at this point, but it most likely has to do with fear of flying off the back end of a machine that uses space and gravity to its advantage to embarrass newbies all across the Tube of You. The meta-analysis also found, not surprisingly, that most people demonstrated decreased endurance on a treadmill vs outdoors. Well obviously, treadmills are boring. This analysis demonstrates that treadmills can throw even trained athletes into a tizzy so if you feel as though you are putting in more effort, you are not alone and don’t assume that perception reflects your training. If you feel that you are putting in less effort, then that can also be normal and I’m jealous. If you are running at faster speeds and are worried about decreased energy expenditure, just increase the treadmill to 1% incline, stop bragging to all your friends and coworkers about your newest PR, and get in your miles.
While treadmills can be a rare form of mental torture, they will not change your form enough to matter, they can be adjusted to reduce lack of air resistance, and they can safely be used to get in some quality training when the great outdoors are just not a current viable option.
Now that I’ve dropped this awesome knowledge bomb on you, click here for more help

You may have heard of the severe health consequences of prolonged sitting. In fact, prolonged sitting has been linked to issues from low back pain to a significant increased risk of death. Some have claimed that sitting is the new smoking. But is it really that bad for you? And if so, what are the solutions?
I’ll explore those issues briefly here.
Some convincing evidence does show a strong relationship to decreased health, including depression, diabetes, heart disease, pain, and death, in those who sit for long periods of time.
I want to focus on the relationship of sitting to the two biggest issues: death and pain. First let’s focus on sitting and mortality.

Multiple studies have investigated the correlation between prolonged sitting and death. These are very difficult studies to perform, because there are so many confounding variables. For example, you can’t just take a group of people, study their sitting habits, measure the rates of death over time, then make a conclusion. For example, how is prolonged sitting measured… by accelerometer or self-report? What if people who sit more are obese, not working, and watch more TV? Maybe it’s those factors, not sitting itself, that is really the problem.
This is just scratching the surface of all the variables to consider. That’s why you have to really look at how the study was done. Also, it takes several studies to often yield a conclusion. I’ll spare you the process of vetting the studies, and instead relay the conclusion from some recent ones that sought to tease out the confounding factors as best as possible.
Last fall, a study from the Annals of Internal Medicine made headlines by showing that there was a direct correlation between time spent sitting and a risk of death, regardless of the cause. Ann Intern Med. 2017.
The researchers tracked nearly 8,000 black and white people 45 yrs and older over four years and noted death rates. The average person sat for just over 12 hrs a day. The longer people sat, the greater the risk of death regardless of the cause, no matter their age, sex, race, body mass index or exercise habits. The big headline from the study showed that even those who exercised did not lower their risk of death if you sat for long periods of time. But it’s important to look at the specifics here.
For example, those who sat for 13 hrs a day had a 200% greater likelihood of death compared to those who sat for 11 hrs a day. What I found particularly interesting is that they didn’t just look at total duration of sitting, but rather at the length of sitting bouts. For example, those who sat for uninterrupted bouts for more than 90 minutes had a 200% greater risk of death compared to those who sat for less than 90 minutes uninterrupted. Those who sat for less than 30 minute bouts uninterrupted had a 55% less risk of death compared to those who sat for bouts greater than 30 minutes.
However, the negative effects of uninterrupted bouts of sitting were not significant for those who were not sedentary (i.e. did not sit for more than 12 hrs a day). So if you aren’t sedentary, bout duration didn’t have a big effect. But if you sit for more than 12 hrs a day, and these bouts are longer than 30 minutes at a time, then your risks of death are even higher.
So what do we know so far about this?
If you sit for long periods of time, try to do it less than 11 hrs a day, and get up and move every 30 minutes. The big part that got the media’s attention was that if you sit more than 12 hrs a day, then go exercise for an hour, it doesn’t negate the risk factors associated with prolonged sitting.
While this is helpful, other studies found that when you more specifically define exercise and the type of sitting (i.e. at work or in front of a TV), stronger conclusions about the role of physical activity were found.
For example, three well-controlled studies of thousands from Briton, Norway, and Denmark (Stamatakis E , et al. Br J Sports Med January 2017. Petersen CB, et al. Br J Sports Med February 2016. Åsvold, B.O., Midthjell, K., Krokstad, S. et al. Diabetologia (2017) showed that prolonged sitting was not correlated with disease or death when obesity and activity was controlled.
A meta-analysis consisting of 16 studies of over a million people showed that in those who were highly physically active (60-75 minutes of moderate to vigorous activity) were able to eliminate the risk of death associated with prolonged sitting, and attenuate the risk of TV watching. They found that those who were not obese, not diabetic, and did not sit > 1 hr a day watching TV, had no increased risks of mortality of disease, even if they sat at work for 8 hrs per day. Biswas A, et al. Ann Intern Med. 2015
The same study did show increased disease and mortality rate for those who sat > 8 hrs / day that were moderately active, and more so for those who were inactive. For these people, prolonged sitting was equal to smoking and obesity as a risk factor for death. Even more interesting was that sitting watching TV was associated with increased mortality compared to sitting doing work.
These studies seem to contradict the conclusion from the first study that regardless of how active you are, prolonged sitting is harmful. However, the first study failed to look at the effects of high activity levels like the previous study. Also, the other studies accounted for the effects of obesity and diabetes. The findings are mostly in agreement when you consider these factors.
So far, here is the take home from the evidence:
Unless you are very active, more sitting increases your disease and mortality risks. Even more so if you are not active. If you are inactive, when you sit for bouts longer than 30 minutes at a time, you have increased mortality risks. Sitting in front of the TV is worse than sitting at work.
Let’s say getting 60-75 minutes of moderate to vigorous activity isn’t a reality for you, and you have a two hour commute each day, and work 8-10 hours sitting at a desk, and God forbid you like to settle in for an hour of Netflix to wrap up your day. This means, like most people, you are at a higher risk of premature death, even if you squeeze in a couple hours of exercise a week.
Given that relocating closer to work and quitting your job isn’t feasible, how about getting a stand up work desk?
Will getting a stand up desk make you more healthy?
Some speculate that decreased calorie burning is why prolonged sitting is so harmful. Accordingly, if people burned more calories, they would have less risk of death and disease. This explains why those who were highly active in the prior studies did not suffer the negative effects of prolonged sitting compared to their less active counterparts.
To follow this line of thinking, researchers would have to prove that standing vs sitting burns more calories. Gibbs, B. et al.( Occup Med (Lond). 2017 Mar) showed that alternating sitting and standing increased calorie burn by 8%, and replacing prolonged sitting with >4hrs of standing increased calorie burn by 11.5%. This could translate to an increase of 57 calories for the average size man.
Another study found that in 15 minutes standing, sitting at a computer, or sitting watching TV you burn 22, 20, and 19 calories respectively. So in 4 hours, you can burn an extra 32-48 calories by standing. The same researchers found you can burn more than that (56 calories) by just getting up and walking for 15 minutes. Creasy S, et al.. J Phys Act Health. 2016.
While it does appear that standing may be a good alternative to prolonged sitting for your health, if its effects are related to burning more calories, its effects are small.
Accordingly, based on the evidence thus far, if you hope to improve your health I would recommend:

This gets a little more complicated.
The biggest reason why is that low back pain isn’t a homogeneous condition. It’s like saying someone has a learning disability. Obviously there are different types, causes, and thus treatments. Unfortunately, no studies have investigated prolonged sitting and its effects on specific types of low back pain. However, using the general classification of low back pain, there does seem to be a strong correlation between sitting and low back pain.
Accordingly, it would seems then that doing more standing instead of sitting is a good option. However, the studies on this are mixed. That is to be expected, because as previously mentioned, low back pain is a multi-factorial issue, one that is likely not to be solved by one intervention. Also, just because prolonged sitting is bad doesn’t mean that prolonged standing is good.
Prolonged anything is in general a bad idea for the human body.
So let’s take a quick look at the science on this.
Several studies have boasted the positive effects of reducing sitting time on back pain. A study in 2011 looked to more directly assess the relationship between the intervention of simply providing desk workers with a sit-stand desk. Twenty-four workers participated in the intervention group, 10 did not, and thus served as the control. (Pronk NP, et al. 2011. Prev Chronic Dis 2012).
Over the next seven weeks, the intervention group reduced their sitting time by 66 minutes per day. The control group increased sitting by 17 minutes per day.
Upper back and neck pain declined in the sit-stand desk group. But, after the seven week experiment was over and the sit-stand desk was removed, the incidence of upper back and neck pain returned.
Interestingly, there was no difference in low back pain or time spent in physical activity breaks between the stand-up desk group and the control group. This means that you can’t credit the improvements to interventions other than the less duration of standing, like being more active.
It was also found that mood improved for the sit-stand group, but these mood improvements were lost once they went back to sitting for two weeks. They also reported feeling more productive, focused, energetic happier, and less stressed. There are some problems with this study, however. First, there were few participants and they were not randomized. Second, all outcomes were self- reported, which may not be reliable. More about this later.
A well-designed study in 2015 gives us some better data to make conclusions about stand up desks and low back pain. (Gupta, N. eta al. PLoS One. 2015; 10(3). The researcher found that among 201 blue collar workers, high sitting time, not just at work (>3.7 hrs.) but also in leisure (>5.4 hrs.), correlated with high low back pain.
This researcher mentioned a very important point that should be appreciated. Their research review identified many studies that showed a correlation between sitting and increased low back pain, and several that showed no correlation. They note that there are several reasons why there may be conflicting findings. The biggest is perhaps that sitting time is measured by self-reports, which could be highly unreliable. However, in this study they used accelerometers to objectively measure activity.
Another factor could be the heterogeneity of the population in terms of socioeconomic factors, which can confound outcomes, as socioeconomic factors tend to correlate with low back pain. However, in this study they attempted to control this factor by only including blue collar workers. In addition, many of these studies did not report leisure time sitting and work related sitting. This could be significant, as overall duration of sitting can vary significantly outside of work. In this case, all workers were blue collar workers, and their sitting time both in and outside of work was assessed via accelerometry
Recently, a meta-analysis was published that concluded the utilization of sit-stand desks does reduce low back discomfort. (Shuchi Agarwal, et al (2018) Ergonomics, 61:4, , ) However, the level of discomfort resolution was low. This was expected, however, because in all of the studies included in the meta-analysis those with pre-existing back conditions were removed from the study. I found this odd because it would be meaningful to see if sit-stand stations were viable interventions for those who are actively experiencing back problems.
Regardless, since meta-analyses are some of the strongest types of research, it’s important to know that this evidence showed a small and significant effect for the sit-stand intervention in reducing low back discomfort.
Unfortunately, the studies included in the analysis used a wide range of sit-stand ratios, thus a specific dosage cannot be recommended.
However, since then a few studies have called into question the utility of standing desks for treating low back pain. In fact, they found using standing desks actually increased low back pain.

Earlier in 2018, Viggiani and Callahan from the University of Waterloo tested 40 adults with no history of low back pain, and 40% of them developed low back pain after standing for two hours but pain dissipated within 10-15 minutes of sitting down. (J Appl Biomech. 2018 Feb 1;34.) This really isn’t that surprising; given some people will have a greater standing tolerance. But, it does give pause to the idea that simply standing is better for back pain.
Also, earlier in 2018 research from Curtin University found that standing desks create discomfort, deteriorating mental reactiveness, and increased ankle swelling. Twenty people were part of the study in which they were exposed to working for two hours uninterrupted while standing. It wasn’t all bad, however, as creative problem solving improved. Richelle Baker, et al (2018) Ergonomics, 61:7,). Again, this isn’t surprising. Few clinicians would advocate for standing uninterrupted for two hours.
Another study with 96 participants found that those who used prolonged standing desks were more uncomfortable, and did not show any change in mood, creativity, or performance. However, they did show greater task interest, enthusiasm, and alertness. Finch, et al. Int j environ res public health 2017.
While it seems like the studies are disagreeing, they really aren’t. They are just highlighting that there are nuances about this topic that can’t be covered inferred from a click bait title in a FB post.
A very recent randomized control trial does a great job exploring the practical use of sit-stand desks by those with LBP, which addresses a problem with the prior studies that I mentioned earlier. (Gibbs et all Occup Environ Med. 2018 May;75(5):321-327)

Researchers looked at the effects of changing sedentary behavior on 27 people with LBP who have desk jobs involving sitting for more than 20hrs/week.
In addition to providing them with sit-stand desk attachment, they were given behavioral counseling, cognitive behavioral therapy for LBP, and a wrist worn activity prompting device.
The intervention group reported a 50% decrease in disability compared to 14% decrease in the control group. As mentioned before, however, there are problems with this study: sitting time was self-reported, and sitting outside of work was not assessed. Also, multiple other interventions were utilized, so we cannot attribute improvements solely to the sit-stand device.
Let’s summarize the evidence about using sit-stand desks for low back pain.
I’ll also throw in my clinical perspective, and wrap this up with combining my overall recommendations of sit-stand desks for both LBP and for general health:
Using sit-stand desks for LBP:
More studies need to be done on those with active low back pain pathologies. Specifically, these studies need to both specify the type of workers and the type of low back condition that they are experiencing.
For example, I’d like to see a study on office workers who baseline sit greater than 25 hrs. a week, measured via an accelerometer (or similar device) who are 35-50 years old suffering from intermittent discogenic, flexion sensitive low back pain treated with a one month intervention of regular physical therapy plus utilizing a sit-stand desk with varying degrees of sit-stand rations, measuring their compliance, and comparing the outcome to those receiving the identical physical therapy, but no sit-stand desk. That would allow us to provide some clear, meaningful recommendations.
Related to the above, we must appreciate that different types of people with different types of back problems are going to respond to different types of treatments related to sit-stand recommendations.
For example:
In all cases, any prolonged positions are not good for your back or your health. Change positions as frequently as possible, and get up and move as often as possible. Ideally, do this every 30 minutes. Don’t confine your options to just sitting or standing. Take a walk. Even better, do a dynamic warm up, or at least components of it. You can do that anywhere, and you don’t need to even leave your work space to do it.
You don’t need further evidence before you act on this advice. Yes, there is seemingly conflicting advice about the use of a stand up desk. There is less conflicting evidence of using a sit-stand workstation. I’ve explained some of the reasons why there is conflicting information above. In light of this lack of absolute certainty, the best way to proceed is to determine: 1. Is it likely to be effective for me? And, 2. Are there significant risks for me? Given that the risks are low or nil (unless you go overboard and switch immediately to standing all day tomorrow) and the benefits are positive, for the majority of people, I advise that they:
If you aren’t sure how the risk/benefit ratio works in your case, please reach out and let me know. As with most things, the goal is not making generalities from the science (that’s what researchers do), but taking the findings and applying it to a specific individual (that’s what coaches and clinicians do). If you are looking for a sit-stand desk, here are a few options to consider:
www.ergotron.com/products/stand-up-desks/desk.conversions,
Michael Stare FOR IMMEDIATE RELEASE
Orthopaedics Plus Physical Therapy
100 Cummings Center Suite 121Q
Beverly, Ma 101915
978-927-2065
Physical Therapy Icon Doesn’t Sell Out, Instead Leaves Legacy and Grows from Within
Orthopaedics Plus Physical Therapy changes ownership, retains founder as a clinical expert.
Burlington, Beverly, MA – When you’ve lead a thriving business for over 30 years in the health care arena, it’s unusual to walk away without being swallowed by the big hospitals or acquired by a large company with hundreds of clinics. Yet, by handing the reigns over to two of their younger clinicians, that’s exactly what co-founders and former owners of Orthopaedics Plus Physical Therapy, Al Visnick, Bill Antonelli, and Vinny Buscemi have done. But they certainly are not going away.
“Our goal was to leave this business as a legacy of what we believe Physical Therapy should be. The ones that I trust to do that are Justin Pezick and Mike Stare, who have the same standards that we have worked hard to create. No large hospital system or multi-region practice would be able to keep that legacy alive” says Visnick, who is guiding the transition process and remains as a treating clinician. “So I’m not going anywhere, I’m just done with the day to day business aspects” clarifies Visnick. Fellow Orthopaedics Plus Co-founders, Bill Antonelli and Vin Buscemi, will continue their roles in managing the physical therapy services for Winchester Hospital’s Outpatient Physical Therapy Clinics.
With offices in Burlington and Beverly MA for 31 and 20 years respectively, Orthopaedics Plus is one of the oldest surviving independently owned PT Clinics in New England. And with 9 of its 13 clinicians possessing between 15-30 years of clinical experience, it’s also one of the most seasoned.
“The 2 biggest factors that made this such a great opportunity to take over ownership is the culture of top-notch patient care that Al, Bill, and Vinny have fostered, and the amazingly talented group of clinicians we inherited” says Dr Mike Stare, who has worked with Orthopaedics Plus for over 14 years as a Physical Therapist in the Beverly office.
As the founder and owner of Spectrum Fitness Consulting for the last 12 years, an award winning personal training studio also in Beverly, Dr. Stare is no stranger to running a business. In his new role as owner of OP, he plans to incorporate many of the lessons he learned growing his fitness studio to his new role as owner of OP. “Helping patients recover is more than making them feel better and get out of pain. It’s about improving their overall wellness and getting to the cause of their issues. Physical Therapy is more than treating knees and backs, it’s about treating people…listening to their goals, caring, and problem solving. To do that, you have to educate them not only when they are patients, but reach out to the community before they are patients.”
Dr. Stare is not shy about reaching out to the community, as he has provided hundreds of seminars and workshops to business, schools, philanthropies, and various groups on injuries, health, and fitness. He also travels nationally teaching thousands of clinicians across the country.
It is the role of educating clinicians that new owner, Dr. Justin Pezick, a clinician in the Burlington office, hopes to continue advancing at Orthopaedics Plus. “OP is responsible for educating many of the top clinicians in New England. Both Mike and I as younger clinicians came to OP earlier in our careers because of their reputation and skill in developing top level clinicians who provide the best care. We have amazing clinicians, and hope to utilize their expertise and experience to continue developing the best clinicians for years to come”.
Dr. Pezick’s skill in modernizing technology and updating billing practices has already paid dividends. “That’s another amazing thing about this partnership transition. Justin has skills and interests that Al and I don’t have, which have already improved operations, profitability, and enhanced patient care” explains Stare.
While Stare and Pezick have taken over OP in January, 2018 with a list of initiatives to enhance the practice, what is most important are the things that won’t change. “Our vision is to keep the key principles intact; retain the most experienced clinicians who get to spend enough time with their patients, something that is becoming less common in PT”, states Pezick. “Furthermore, Al Visnick will remain as a clinician and Director of Treatment in Bulrington, continuing to treat patients in the Burlington clinic. In addition, Ellen Poveromo will remain as the Director of Treatment in the Beverly clinic. Al and Ellen are such an important assets, so retaining them as expert clinicians is something we are thrilled about.”
Dr. Pezick, who also shares a similar background in fitness as his new partner, aims to expand upon the traditional role of Physical Therapy care. “To address the goals of patients, we need to go beyond rehabilitation, and incorporate wellness into the clinic.” With expertise in Athletic Training, Strength and Conditioning, nutrition, and fitness, along with fellowship training in manual therapy, the new owners are well poised to introduce these practices into their clinics. “We have an all-star staff, each who have exceptional expertise beyond general orthopaedics and spine care including pelvic floor dysfunction, scoliosis management, weight loss, post-masectomy care, athletic performance, and more” adds Stare.
While most of what Orthopaedics Plus is known for will remain the same, the new owners do have changes in mind. “The change current and returning patients will notice most is an upgrade in the physical clinic in Burlington.” says Pezick, who is planning renovations to be ready by the end of the year.
“In addition, we strive to make the following changes: 1. Dramatically increase awareness in the Beverly, Burlington, and surrounding communities of our unique and advanced care opportunities. 2. Expand opportunities for clinicians to further develop their clinical expertise through providing specialized care and education programs and 3. Advance our clinical education program to develop and train clinicians seeking advanced post-doctorate specialization.” States Stare.
“Our goal is not primarily to grow through expanding clinics across New England. Rather, our goal is to focus our efforts to be the most effective, sought-after provider for physical therapy. And we want to be the place where top level clinicians who love what they do come to learn, and stay to treat for the rest of their careers. That’s the formula we’ve seen last through decades of treatment trends and health care changes to best help patients.”
With the new ownership at the helm and Visnick in the clinic, he’ll have a great perspective to see his legacy plan unfold with Orthopaedics Plus. “I think we’re well poised to be around for another 30 plus years.” Says Pezick.