Chances are you or someone you know has dealt with sciatica. This is a condition when you have pain; be it sharp, dull, or tingling, that shoots from your rear, down the back of your thigh, or down your leg.
Unfortunately, this condition is poorly managed. As a result, it needlessly wreaks havoc on people's function, fitness, and can contribute to unnecessary pain, disability and exposure to risky treatments.
The usual treatment for this condition is all over the place:
- See your PCP, and take some medicine – usually some type of muscle relaxant or anti-inflammatory
- Wait it out and hope it goes away
- Do some stretching for your "tight" back, hamstrings, or "piriformis" muscle
However, these treatments are not usually effective or supported by the evidence. And a recent study further clarifies this.
The evidence shows that physical therapy consisting of exercise and manual therapy is significantly more effective.
Before we delve into the evidence and best treatment options, let's get a deeper understanding of sciatica.
What is sciatica?
Sciatica refers to a condition that causes pain from your low back to your buttock, posterior thigh, and leg. These symptoms are attributed to an irritation of the largest nerve of the body, the sciatic nerve. This irritation can be from inflammation, compression, or excessive tension applied to the nerve.
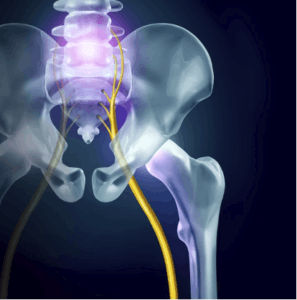
Damage to structures adjacent to the sciatic nerve or its associated nerve roots, such as spinal structures or hip muscles, are suspected culprits for contributing to the nerve irritation. However, this is conjecture, and no imagine can confirm the exact mechanism of the irritation. This partly explains why approaches trying to target a specific part of the anatomy have very poor success rates.
It's quite a frustrating condition that can linger for weeks or months without proper treatment and can wreak havoc on your function and fitness goals.
What's the first thing to do if you have Sciatica? The Recent Evidence
Researchers recently investigated whether the usual course of care or physical therapy was more effective in treating sciatica. 220 people presenting to a primary care setting with sciatica lasting less than 90 days were randomly assigned to one of 2 groups. Group one received the usual care, which involved education and medication (anti-inflammatories and muscle relaxants).
The other group received 4 weeks of physical therapy, which consisted of exercise and manual therapy. At 4 weeks, the physical therapy group demonstrated superior outcomes. 1 year later, the physical therapy group continued to show lower levels of pain and disability. Fritz, JM et al. Physical Therapy Referral From Primary Care for Acute Back Pain With Sciatica A Randomized Controlled Trial. Annals of Internal Medicine. Oct 2020.
These findings tell us what my colleagues and I have known from treating hundreds of patients with sciatica: those who get physical therapy do better than managing it with medication. And the earlier sciatica patients receive PT, the better.
How to Fix Sciatica
Here are the steps I have found, based on the evidence, being a patient with sciatica, and treating hundreds of patients with sciatica for the last 2 decades has been most effective in fixing sciatica;
1. Make a PT appointment
The research above confirms what other studies have found: early PT improves outcomes. Evidence also shows that early PT also lowers the risk of surgery, reduces costs, and lowers the likelihood of using addictive pain killers. But there is another important benefit: getting a proper diagnosis. Sciatica, like many back issues, can be difficult to diagnose. No matter how skilled the clinician, having only 15-30 minutes on one day to evaluate a condition is challenging. In contrast, seeing how your condition responds over time on different days to various movements and treatments is essential to confirm a diagnosis. This is not possible in environments other than physical therapy, where you are seeing a Doctoral trained clinician for 30-60 minutes several times a week.
We can gather critical information to make sure we are treating the right condition. For example, many people have been sent to me with a diagnosis for calf muscle strains, hamstring injury, or knee arthritis, only to find out that upon PT examination these were sciatica cases. In other situations, we've seen people referred to us for sciatica and low back pain that were not responding as expected to treatment and examination revealed inconsistent findings.
This information allows us to send the patient back to his PCP with justification to explore non- orthopedic causes of their pain. In 2 such instances, it was determined that their back and leg pain was referred from having kidney stones. The most supported PT treatment involves exercise, manual therapy, and education. Thus, PT's who specialize in this treatment approach, versus passive modalities only (e-stim, ultrasound, stretching) are best to treat sciatica.
2. Stop stretching.
One of the biggest mistakes in treating sciatica involves stretching the hamstrings. Nearly all sciatica patients that I'm seeing as a second opinion due to failure to respond to prior treatment notice that their pain improves within days with advice to stop stretching their hamstrings. Because the hamstrings are often tight and are located near the path of the sciatic nerve in the back of the thigh, many clinicians and patients alike believe that this tightness is causing their sciatica. Accordingly, they think stretching the hamstring will help. However, this often makes it worse because muscle and nerve react quite differently. While a muscle will tolerate stretching quite well, an irritated nerve will not.
Doing so is like adding gas on a fire. While some may report that stretching actually feels good, this is only temporary and can create a vicious cycle. The sense of stretch may create a diversionary symptom that drowns out the sciatic symptoms, but then later return and the hamstring muscles often tighten as a guarding response. This is similar to stretching an itch: it may provide temporary relief, but it often causes skin breakdown and elevates histamine that fuels the itching sensation. This is similar to stretching the piriformis, a hip muscle that is located near the sciatic nerve as it passes the buttocks.

In about 20% of the population, the sciatic nerve passes straight through the piriformis muscle. Somehow, this has led clinicians to suggest stretching the piriformis to treat sciatica. However, a close look at the mechanics of the piriformis stretch would reveal that stretching this muscle would add tension and compression to the nerve, as opposed to relieving it. Also, there is no proof that piriformis tightness, nor stretching that muscle, relieves sciatic symptoms.
Given that both of these suggestions lack support and have a high likelihood of worsening symptoms, avoiding these stretches when the sciatic nerve is irritated is an excellent first step. While these stretches may be tolerated later as the sciatic nerve calms down, doing so while the nerve is aggravated is not advised.
3. Change ergonomics
Given that prolonged tension or compression on an irritated nerve will often prolong irritation, these positions need to be identified, then modified or avoided. Common positions are sitting up in bed or sitting with the feet elevated on an ottoman. These positions increase the tension of the sciatic nerve and will often flare up symptoms. Sometimes prolonged standing will also aggravate sciatica, which is common when there are sensitivities to compression. This is best modified by doing intermittent traction while standing, weight shifting, or minimizing uninterrupted prolonged standing.
4. Make a provocation/Alleviation list
Knowing exactly what increases your symptoms and decreases your symptoms is vital information. Having it in list form can make a seemingly mysterious condition appear much more manageable. This serves as your reminder for what you need to address in order to solve your sciatica condition. If you do the correct treatments but fail to change the thing that are making your pain worse, it can be like taking Tylenol for a headache, then banging your head on a wall.
5. Make a modify/avoid/do list
This directly relates to the above. For the things that you have identified as provoking your pain, you need to decide if you can avoid them until things calm down or not. If you can avoid them, then do so. But if these things are unavoidable, then they need to be modified. For example, if sitting provokes your pain, but you need to sit for work or commuting, then change your chair, take more frequent standing breaks, or do intermittent deloading while you sit. These are the things that get overlooked in treatment, but probably make the biggest difference in outcomes.
6. Get a neuro exam
If a nerve root is affected as it exits the spinal column, its function can be compromised. While symptoms radiating down the leg may be one clue that the nerve may be affected, it is not a very reliable finding. This is because irritation of several other structures of the spine may also refer pain down the leg. Imaging, such as MRI, is also a flawed way to determine the involvement of nerve irritation, as many people without any pain or dysfunction have MRI findings of herniation or "nerve compression".

However, a neuro exam may be a better indicator of the status of how the nerve roots as they exit the lower lumbar spine are functioning. A neuro exam involves testing three important functions of a nerve root: motor (strength), sensation (touch, temperature), and reflexes. Each nerve root is responsible for the function of specific muscles (myotomes), area of skin (dermatome), and specific reflex (Deep tendon reflex). This is really important as it can identify if a nerve root is involved, how severe the involvement is, and whether it is improving or not over time. For example, if a patient presents with weakness of his tibialis anterior (the muscle that pulls your foot up), decreased sensation on the inside of the shin, and a diminished patella reflex, then it is likely that the L4 nerve root is affected.
If these signs become more severe over time, it increases the rationale to consider more aggressive treatment to prevent permanent nerve damage. While this is rare, it is vital and may prevent permanent impairment. Conversely, improvements in the neuro exam findings, even in the absence of improved pain, can serve as a positive indicator of potential for future improvements. This is important as it can prevent people from giving up on conservative treatment or seek risky and unnecessary treatment.
While many clinicians do rough neurological assessments (having you walk on your toes, then heals, then hitting your patella with a reflex hammer) a thorough neuro exam is more involved and uses a grading system to detect more nuanced changes. Also, a neuro exam should be done not just once, but several times as the condition may change and detecting these changes early are important. A physical therapist with residency or fellowship training in spine care is best to perform a neuro exam, as they have the training and time to perform more frequent and thorough neuro exams.
7. Determine sensitivity to tension, position, or load.
Understanding your sensitivity to these 3 things will greatly help guide treatment and resolution of your sciatica. This is best done during a PT exam. Tension sensitivity: tests that evaluate the response of the nerve tissue to stretch can help make the diagnosis more accurate. For example, a slump test may help distinguish between a hamstring injury versus sciatic nerve irritation. It can also help measure the rate of improvement and guide decisions about when to resume normal activity.
Position sensitivity can help determine which activities to modify or avoid, and which type of exercises to pursue. This can make or break the success of treatment.
Finally, assessing load sensitivity can be critical for acutely reducing symptoms, and may hasten recovery. For example, if a patient is determined to be load sensitive, doing traction in the clinic and teaching you how to perform self-traction can be the difference between a bad day in pain versus getting significant relief. Some evidence indicates it may improve the fluid dynamics and nutrition of the disc as well.
8. Identify risk factors
Individual risk factors that you can modify may make you at risk for various back problems, and thus could be contributing to the cause of your back pain. Finding these risk factors and improving them can be important for not only recovering from sciatica, but also for preventing it from coming back. For example, impairments with motor control, endurance, strength, mobility, and general fitness can be contributing factors that are easily improved with proper care.
9. Understand pain
Too many people fear pain or ignore pain. Both extremes are rarely successful. Understanding what pain is can greatly improve your ability to manage your sciatica. For example, knowing that the severity of pain does not always correlate with the severity of damage can prevent you from pursuing unnecessary, ineffective, or dangerous treatments. Pain education is a critical element of proper treatment.
10. Stay Active

It may sound counterintuitive, but one of the most important things to do when you have any back condition is to remain active, as complete rest has been proven to negatively effect outcomes. The trick is to figure out the right type and amount of activity. Too much of the wrong things will aggravate the condition, and too little will do the same through increasing tissue sensitivity and lowering resilience. We need to find the "goldilocks zone".
Staying active will not only help your condition improve, but it is absolutely vital for your general physical and mental health. An injury is a reason to move, not a reason not to move. The key is finding the right type and amount. As a patient, it is hard to be objective about this, thus, having the support of a clinician is key.
What to do next
Get help from a trained clinician with experience in treating and preventing back problems if you have been dealing with sciatica symptoms. In most cases, this means seeing a residency or fellowship trained physical therapist. Click here to schedule an exam, or learn more about our clinicians. If you aren't in the area, this can at least give you an idea of the background that I would look for when choosing a PT.
A personal trainer or fitness coach experienced in working with post-rehabilitation will also be a good resource. Especially if you have had chronic back or sciatica problems that have been successfully managed in PT, but you would like to get in better shape and aren't sure what you can do without provoking your back problem. Click here to set up a consultation.
Sciatica can be a frustrating condition and having so many different treatment options and opinions can make it more challenging. Fortunately, focusing on the evidence and following success clues from the clinic is a good reason to be optimistic for a full recovery. Hopefully the information above gives you some good first steps as to what to do to help your sciatica!
