Core
Gluteus Medius
Calves
Quads
Gluteus Maximum and Hamstrings
Core
Gluteus Medius
Calves
Quads
Gluteus Maximum and Hamstrings
Are you in constant or recurring pain that will not let you enjoy your life as you would like? Do you suffer from the effects of an old injury, a degenerative condition, or some other situation that calls for ongoing pain management? If so, then your first instinct might be to reach for medication — but hold that thought, because drugs can pose their own threats to your health. Physical therapy can provide safer, effective, non-addictive, long-lasting strategies to manage pain.

Drugs promise quick (if only temporary) relief from many kinds of pain. Unfortunately, they can harm as well as help. The most glaring example is the addictive potential of opioid drugs. Opioid dependence and abuse have become a national nightmare in the last decade. The CDC estimates the total economic burden of prescription opioid misuse alone in the US is $78.5 billion/year including the costs of healthcare, lost productivity, addiction treatment and criminal justice involvement. Some researchers even feel that many people who would otherwise be able to work are sidelined because they would fail a drug test. Roughly 21-29% of patients prescribed opioids for chronic pain misuse them. Between 8-12% develop an opioid use disorder. An estimated 4-6 % who misuse prescription opioids transition to heroin. As mind-blowing as these numbers are, to a person who uses prescription pain medication for pain relief, opioids may seem like the path of quick recovery. The misuse of opioids remains a problem in our society. The key is to seek help before pain gets out of control.
Even over-the-counter pain relievers can pose dangers to your health. Taking painkillers to rid yourself of pain may seem like a good solution, but it is not. Over-the-counter meds like aspirin, ibuprofen and acetaminophen can have side effects. Taking a lot of aspirin can cause your stomach to bleed and can also cause kidney damage. Acetaminophen can result in kidney damage. Ibuprofen can cause both kidney and stomach problems. Not only does taking meds for pain just mask the problem, it may cause you another one. Using medication for pain does not get to the root of the problem. None of these medications are meant to be used long term. Pain is not supposed to linger.
Pain is your body’s natural warning system — which makes it a particularly important and useful communication tool at early onset of injury. Nerve signals alert you to a problem that requires attention, from an infected area or traumatic injury to joint or overuse of a muscle or tendon. This is especially true of acute pain. Sensations of pain and stiffness discourage you from using an injured body part while it is healing; once the condition resolves, pain should go away.
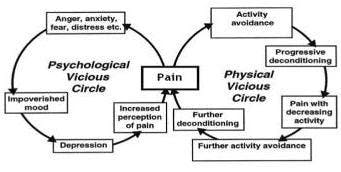
When pain does not go away, it is important to investigate why. Sometimes pain will outlive its usefulness, lingering on for months or even years after your body has done all it can to address the underlying problem. We call this chronic pain. It afflicts some 116 million people in the U.S. alone, that is 1 in 10 people suffer from chronic pain. The pain may plague you constantly, or it may come and go in bouts that last for weeks at a time. We have a quick fix culture and physicians yield to meeting patient’s demands for passive prescriptive treatments. The solution is not to repeatedly mask pain with medication and put off the need to address why your body is trying to tell you something. Pain and suffering are the primary reason American’s are on disability. This vicious cycle is because the root causes of pain are left unaddressed. As the opioid epidemic has inflicted the US and healthcare professionals are seriously reevaluating its abuse, it is worth noting that PT has long been considered a safer, cheaper, and more effective treatment for chronic pain.
Physical therapy not only can help relieve pain; it addresses what is causing the pain in the first place. A physical therapist is a highly trained medical professional, and an expert in the biomechanics of movement. Through advanced diagnostic procedures, a physical therapist can uncover the source of your pain and find ways to address it for long-term health and mobility. Our healthcare mindset needs to shift. Physical Therapy should be a first line response to pain. A physician will outsource your needs, whereas a PT will help you take charge of your own care.
The focus of treatment should be to restore function disability not just treat pain symptoms alone. This would make the 1/3 US population much more productive and living a better life without paying the price of drugs. Physical Therapists are in a prime position to guide a person who is suffering from pain, disability and struggling with the social, psychological, and even economical stressors that accompany pain. Treatment addresses the physical and psychological challenges a patient is faced with when trying to get their life back. Clinicians address a patient’s individual concerns and apprehensions with weekly support and coaching, keeping a person on track with necessary lifestyle changes that will empower an individual to take control of pain while restoring physical function. Careful exposure to exercise and activity while keeping symptoms at a minimum permits a person to discover how physical activity can be a path and even the reward to relieve pain.
Stay tuned for additional information about the integrative science of pain. If you’ve ever experienced a disabling injury it would behoove you to know what is the difference between acute and chronic pain, learn about the psychological components of chronic pain, and discover how a person who has learned how to avoid physical activity because of pain, can take control over pain and return to a more productive life.

If you are a runner, you are probably overjoyed by the fact that you are still able to safely run during the COVD-19 pandemic. Not only are you able to run, you are actually encouraged to do so as it is important not just for your fitness, but also your immune and mental health.
Your running, however, has probably changed:
While running is still allowed, it has changed.
“It is not the strongest of the species that survives, nor the most intelligent that survives. It is the one that is most adaptable to change.”
-Charles Darwin
With all of the current changes to your running, this may be a perfect opportunity for you to make additional adaptations to not just survive, but to thrive.
If you have a chronic, low grade injury that tends to flare up with an increase in intensity or mileage, this may be the time to do something about it.
Maybe you’ve always wanted to learn how to become a more efficient or faster runner?
Possibly you’ve heard that you should be doing strength training but you’re just not sure what you should be doing.
Luckily for you, OP is here to help.

Through Limitless Running, we have both in-clinic and virtual options to perform a gait analysis that will identify the problem areas in your running form. With follow up visits including gait retraining to correct your form and a re-assessment to ensure that you are on the right track, we’ll be able to help you get back to running without injury and with improved efficiency.
Our highly trained physical therapists are also runners who enjoy spending their free time geeking out over the optimal knee bend during initial contact and what percent of running cadence increase has been shown to be most beneficial in the newest systematic review. They have a plethora of information to share with you and encourage you to pick their brains.
If you would like to learn more about our new program, head to our webpage here.
Quick Facts:
From my experience, both as a long distance runner and a physical therapist, getting runners to perform strength training is similar to getting a picky 3 year old to eat raw broccoli. Not easy. Personally, I do not enjoy strength training. Tell me to go spend 5 hours alone on a technical trail in 40 deg weather with pouring rain and gusting wind – no problem. Ask me to spend a total of two sessions in a gym per week and I will revert back to my 3 year old self and stare you right in the eye as I intentionally drop my broccoli onto the floor.
Based on these opinions, I was excited to read an article by the PT running goddess, Irene Davis, that explained that strengthening, specifically hip strengthening, has no effect on running form. Her article demonstrated that although strengthening the hips of runners with poor form improves hip strength (obviously) and performance of a single leg squat (similar to landing position of running), there was no change in the participant’s running pattern. After reading this, I smiled, high fived myself, and began dreaming of a life without gym bros. Kidding.
Then why strengthen?

While Willy & Davis, Feber, and Earl & Hoch, have demonstrated that just strength training alone is not enough to improve poor running form, strengthening does have its place in the world of running. Most notably, it can do wonders for preventing injury and making you faster. If you strength train (and eat your raw broccoli), you’ll never be injured again and you will win all of your races. Kidding again.
Realistically, strength, or lack thereof, has been shown through a plethora of studies to be associated with injury rates. A too-close-to-home one includes a systematic review that demonstrates that females with patellofemoral knee pain (generalized front of the knee pain) are found to have weaker hips. This corresponds with other studies that demonstrate that females with patellofemoral knee pain are found to run with aberrant hip mechanics such as this:
The working theory is that weakness will lead to faulty gait mechanics (running form) which will then lead to injury. Pretty solid.
Why, then, is just strengthening often not enough? If we get stronger, shouldn’t our gait mechanics also improve?
If only it were that easy. Research has been able to clearly demonstrate that weakness can lead to poor running form which can lead to injury, but once those running mechanics become our new pattern, they are not easily changed.
Think back to your most recent vacation. Without an early morning work meeting requiring you to set an alarm, you may have gone to bed a little later than usual on the first night smiling at the fact that you get to sleep in. As the vacation continued, that bedtime probably crept further into the night and that sun continued to rise higher in the sky before you opened your eyes. All was well and good until back-to-reality Monday morning hit and you had to hit snooze three times and lower your personal hygiene standards in order to make it into work on time. Falling into that new sleeping schedule was easy, climbing back out of it – bit of a challenge.
Just as it often takes different and more difficult steps to revert back to your normal sleep schedule after a vacation of late nights, improving your gait mechanics after injury requires a bit of effort. Strengthening will help. Specific drills and strategies to improve running form can assist. But just as Davis demonstrated, we need more than that.
We need gait retraining.

Gait retraining is simply an umbrella term used to describe ways in which we can change running form and it has been shown time and time again to improve your running pattern, rid yourself of injury, decrease total load on your joints, and increase your performance. Gait retraining typically falls into two different categories, visual and auditory. Visual gait retraining can include placing a mirror in front of your treadmill to watch yourself run with special markers and tricks. Auditory retraining is very commonly prescribed as running to a metronome or listening to the sound of your footfalls (with specialized equipment). While some of these tools may be helpful to you, determining which one will help and how to use it appropriately needs to be prescribed by a medical practitioner who is trained in performing a gait analysis. This is a PLEASE REACH OUT TO AN EXPERT warning with a caveat that knowledge is power so you can also learn more about gait retraining here.
During the COVID pandemic, we are currently offering in-clinic and virtual gait analysis with assessment and follow up sessions to safely and effectively provide gait retraining to injured runners. If you are interested in learning more, please click here for more help or give us a call at 978-927-0907

Quick facts:
When you feel that faint tug on your kneecap as you descend a set of stairs after a challenging run, are you haunted by that whisper in your ear, “running is bad for your knees?” As an ultra runner and physical therapist, that voice in my head has been strengthened by numerous friends, family members, and even patients who try to warn me that I’ll be facing a world of pain when I’m older if I keep up this “crazy running” thing.
My reply is generally two fold:
Well, fortunately and unfortunately (who likes to be wrong?), I have been responding incorrectly. My “educated decision” did not include new evidence that has emerged indicating that not only is running not related to knee osteoarthitis, it may actually be protective for your knees.
Here’s the old thought process: Running involves a lot of pounding, pounding causes damage, therefore, by the transitive property, running causes damage. Don’t worry, I’m not making an argument against the transitive property (it’s maybe the only part of geometry that I remember from Mr. Lindahl so I’m holding onto it), I’m just no longer convinced that pounding causes damage.
“Damage” or degradation of the cartilage in your knee leads to osteoarthritis. Signs of osteoarthritis can be determined by a few different mechanisms, two of them being the level of cytokines and COMP in your synovial fluid. Okay, okay, let’s back up and define. Your synovial fluid is the fluid inside all of your joints that provides nutritional support for your cartilage and reduces friction. This synovial fluid contains COMP or cartilage oligomeric matrix protein that is a marker for worsening osteoarthritis. This fluid also contains cytokines which are proteins secreted by the immune system that are a sign of inflammation, which is chronically high in patients with osteoarthritis. Basically, high levels of COMP and cytokines are bad news for your knees.

Based on the old thought process, one would expect that runners have relatively higher amounts of COMP and cytokines in their knee joint synovial fluid because people assume that running causes osteoarthritis. However, a new study conducted out of Provo, Utah looked at these two proteins, COMP and cytokines, in volunteers after they had been sitting for 30 minutes or running for thirty minutes. To the glee of all runners, this study found that the levels were HIGHER than baseline in the volunteers after they had been sitting and LOWER than baseline values after they had been running.
Therefore, running may actually protect your knees from osteoarthritis.
Before you text an “I told you so” to all of those NARPs (non-athletic regular person) who have ever questioned your running obsession as you throw on your running shoes and race out the door, here are a few things to keep in mind:

While no other studies solve these issues with analysis of COMP and cytokine levels, luckily, these are not the only scientists who have studied osteoarthritis and running. An article from 2009 looked at long-distance runners over the age of 50 who had already been running for about a decade and matched them with similarly aged participants who did not run. After Xraying these folks every few years for the next decade, there was no difference in the acceleration, prevalence, or severity of osteoarthritis between those who ran and those who didn’t. In fact, the only knee replacements that were performed between these 98 participants were non runners. PLEASE do not infer from that statement that no runner will ever require a knee replacement.
Other grains of salt regarding that study include that the runners group had a lower BMI (higher BMI is associated with increased risk of osteoarthritis), were slightly younger, and had a greater prevalence of prior knee injuries. While all of these values were statistically non-significant, (i.e. age of runners: 59.8 vs age of controls: 60.2), they should be kept in mind. Another key quality of the study to consider is that osteoarthritis was determined through radiographic imaging, yet we have a ton of evidence that demonstrates that Xrays do not always correlate with symptoms. Just because a runner’s Xray doesn’t look too shabby, doesn’t mean that runner is pain free in the knees.

While, as always, more studies should be conducted to look at the long term effect of running on knee OA, I’ll leave you with some statements from oldie but goodie articles:
“Our observations suggest, within the limits of our study, that long-duration, high-mileage running need not be associated with premature degenerative joint disease in the lower extremities”
And
“In sum, habitual physical activity does not increase the risk of knee OA for men or women.”
I’ll make sure to hear these voices in my head next time my knee complains on a stair 🙂
If you want to learn more, click here

Quick Facts:
As spring weather begins to tease with occasional days of sunshine and warmth, the call to run in the great outdoors reaches its peak. After experiencing a run filled with breathing in your own hot phlegm that’s stuck to your mask and dodging the newcomers who have discovered your favorite running route, you may find yourself opting for indoor exercise and instead, pumping out seemingly endless miles on a dreadmill – sorry, sorry, treadmill. While this can allow you to get in a solid training run devoid of any potential pandemic threat, there are a lot of questions surrounding the belted beast. Will running on a treadmill vs running outside change your form? Is the old 1% incline rule real? Why is it so freakin’ hard?
Will running on a treadmill vs running outside change your form?
A bit. Does it matter? Not so much. KINETICally speaking (think force or load on joints), there is a slight difference in the amount of load on your muscles and tendons as you run on a treadmill versus running outside. A recent study shows that your quadriceps muscles can work as much as 27% LESS on a treadmill versus outside, formally called overground. If you are training for a (likely virtual) hilly race, make sure you supplement your treadmill training with some eccentric quadricep training to prevent quad explosion on the downhills. On the flip side, your achilles tendon (the thick tendon that connects your calf muscle to the back of your heel) undergoes up to a 14.2% increase in stress on the treadmill versus the great outdoors. If you suspect that you’ll be spending a chunk of this pandemic on a treadmill, make sure to get your achilles ready with some calf raises.

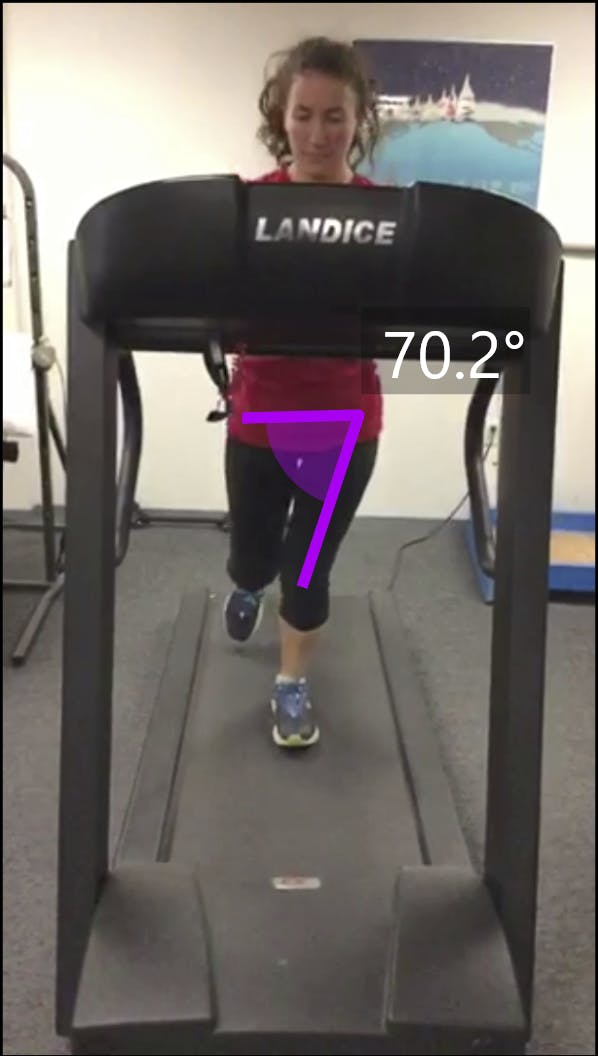
How else does your running form change? KINEMATICally speaking (think position of joints, not force), your hips, knees, and ankles hit pretty much the same angles when you run on a treadmill versus overground. A recent – excuse me – very recent, meta-analysis found that the only difference on treadmills is that when your foot hits the ground, your toes tend to land a little closer to the ground (less dorsiflexion) and your knee has a bit more bend (more flexion). This corresponds with a step length difference of 1-5% which generally indicates that your initial contact (when your foot hits the ground) is closer towards your center of mass (more underneath your body). PHEW. Just look at the pictures.

Fine? Better!
Except that they suck. I don’t think I am alone in feeling as though each mile run on a treadmill deserves a medal in itself as the miles – no – the 0.1 miles, tick by ever so slowly.
So is running actually more difficult on a treadmill?
No. In reality, according to a commonly cited , if you are running anything faster than a 7 minute mile, you should actually increase the treadmill to 1% incline to make up for the lack of air resistance. And if you can get up to around a 5 minute mile, you may even want to increase it to 2%. Yikes.
Despite the fact that running on a treadmill requires less energy due to the lack of air resistance, this meta-analysis found that when running at faster speeds, your heart rate and perceived level of exertion are higher on a treadmill than if you are running that same fast speed overground. Conversely, when running at slower speeds, your perceived level of exertion and your heart rate are decreased on a treadmill versus running that same slow seed outdoors. Kinda weird. We can only speculate at this point, but it most likely has to do with fear of flying off the back end of a machine that uses space and gravity to its advantage to embarrass newbies all across the Tube of You. The meta-analysis also found, not surprisingly, that most people demonstrated decreased endurance on a treadmill vs outdoors. Well obviously, treadmills are boring. This analysis demonstrates that treadmills can throw even trained athletes into a tizzy so if you feel as though you are putting in more effort, you are not alone and don’t assume that perception reflects your training. If you feel that you are putting in less effort, then that can also be normal and I’m jealous. If you are running at faster speeds and are worried about decreased energy expenditure, just increase the treadmill to 1% incline, stop bragging to all your friends and coworkers about your newest PR, and get in your miles.
While treadmills can be a rare form of mental torture, they will not change your form enough to matter, they can be adjusted to reduce lack of air resistance, and they can safely be used to get in some quality training when the great outdoors are just not a current viable option.
Now that I’ve dropped this awesome knowledge bomb on you, click here for more help